Pemphigus Case Study
Pemphigus
A rare group of blistering autoimmune diseases that affect the skin and mucous membranes
Autoantibodies form against desmoglein.
Desmoglein forms the “glue” that attaches adjacent epidermal cells via attachment points called desmosomes.
When autoantibodies attack desmogleins, the cells become separated from each other and the epidermis becomes “unglued”, a phenomenon called acantholysis.
This causes blisters that slough off and turn into sores. In some cases, these blisters can cover a significant area of the skin.
PEMPHIGUS VULGARIS (PV)
![]()
The most common form of the disorder and occurs when antibodies attack Desmoglein 3.
Sores often originate in the mouth, making eating difficult and uncomfortable.
Although pemphigus vulgaris may occur at any age, it is most common among people between the ages of 40 and 60.
It is the most common subtype of pemphigus, accounting for 70% of all pemphigus cases worldwide
CASE STUDY EXAMPLES


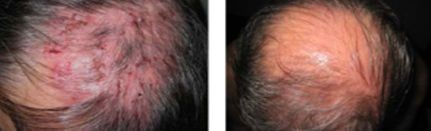
PEMPHIGUS FOLIACEUS (PF)
![]()
The least severe of the three varieties.
Desmoglein 1, the protein that is destroyed by the autoantibody, is found in only the top dry layer of the skin.
PF is characterized by crusty sores that often begin on the scalp, and may move to the chest, back, and face.
Mouth sores do not occur. It is not as painful as pemphigus vulgaris, and is often mis-diagnosed as dermatitis or eczema
Although pemphigus vulgaris may occur at any age, it is most common among people between the ages of 40 and 60.
It is the most common subtype of pemphigus, accounting for 70% of all pemphigus cases worldwide.


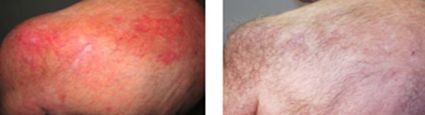
IMMUNOGLOBULIN A (IGA) PEMPHIGUS
![]()
A group of newly characterized immune-mediated intraepidermal blistering skin diseases.
Unlike typical immunoglobulin G (IgG)–mediated pemphigus, IgA pemphigus is characterized by tissue-bound and circulating IgA autoantibodies that target the desmosomal proteins of the epidermis.
SIGNS AND SYMPTOMS
Mucous membranes
Mucous membranes of the oral cavity are involved in almost all patients with pemphigus vulgaris.
Patients may have ill-defined, irregularly shaped, gingival, buccal, or palatine erosions, which are painful and slow to heal.
Erosions may be seen on any part of the oral cavity, and they may spread to involve the larynx, with subsequent hoarseness.
Other mucosal surfaces may be involved, including the conjunctiva, esophagus,, urethra, nasal mucosa, anus, and male/female genitalia.
Skin
Primary lesion of pemphigus vulgaris is a flaccid blister filled with clear fluid that arises on healthy skin or on an erythematous base.
Blisters are fragile and may rupture, producing painful erosions (the most common skin presentation).
Nails
Acute or chronic paronychia, subungual hematomas, and nail dystrophies affecting one or several fingers or toes have been reported with pemphigus vulgaris.
DIAGNOSIS
Pemphigus is also commonly diagnosed by physicians specializing in ENT, oral, or ocular medicine, as lesions can affect the eyes, throat, and mucous membrane of the oral cavity.
Definitive diagnosis requires examination of a skin or mucous membrane biopsy by a dermatopathologist or oral pathologist.
The skin biopsy is taken from the edge of a blister, prepared for histopathology and examined with a microscope.
Definitive diagnosis also requires the demonstration of anti-desmoglein autoantibodies by direct immunofluorescence on the skin biopsy. These antibodies appear as IgG deposits along the desmosomes between epidermal cells, a pattern reminiscent of chicken wire. Anti-desmoglein antibodies can also be detected in a blood sample using the ELISA technique.
Half of people with pemphigus have mouth lesions alone during the first year but develop skin lesions later.
PHYSICIANS
Research
Ahmed AR, Spigelman Z, Cavacini LA, Posner MR. Treatment of pemphigus vulgaris with rituximab and intravenous immune globulin. N Engl J Med. 2006 Oct 26;355(17):1772-9.
Ahmed AR, Shetty S. A comprehensive analysis of treatment outcomes in patients with pemphigus vulgaris treated with rituximab. Autoimmun Rev. 2015 Apr;14(4):323-31.
Ahmed AR, Nguyen T, Kaveri S, Spigelman ZS. First line treatment of pemphigus vulgaris with a novel protocol in patients with contraindications to systemic corticosteroids and immunosuppressive agents: Preliminary retrospective study with a seven year follow-up. Int Immunopharmacol. 2016 May;34:25-31. doi: 10.1016/j.intimp.2016.02.013
Definitive diagnosis requires examination of a skin or mucous membrane biopsy by a dermatopathologist or oral pathologist.
The skin biopsy is taken from the edge of a blister, prepared for histopathology and examined with a microscope.
Definitive diagnosis also requires the demonstration of anti-desmoglein autoantibodies by direct immunofluorescence on the skin biopsy. These antibodies appear as IgG deposits along the desmosomes between epidermal cells, a pattern reminiscent of chicken wire. Anti-desmoglein antibodies can also be detected in a blood sample using the ELISA technique.
Half of people with pemphigus have mouth lesions alone during the first year but develop skin lesions later.